Skin cancers of the eyelid
Skin cancers can occur anywhere on the body but are most commonly found in areas which are exposed to the sun. This includes the face and the eyelids. About 10% of all skin cancers occur in the eyelids.
There are many different types of eyelid cancers, but the 3 most common ones that occur in the skin of the eyelid are the:
- Basal cell carcinomas (BCC)
- Squamous cell carcinoma (SCC)
- Melanoma
The BCC is the most common skin cancer of the eyelid. SCC is less common, and melanoma is rare in the eyelid.
Sun exposure (UV light) is the main risk factor for eyelid skin cancers. People who have spent a lot of time in the sun during their lives are most at risk. People with fair-skin are more at risk.
Other rare factors that may put a person at risk of skin cancer of the eyelid include previous radiation therapy, immunosuppression therapy for other cancers, and certain genetic syndromes.
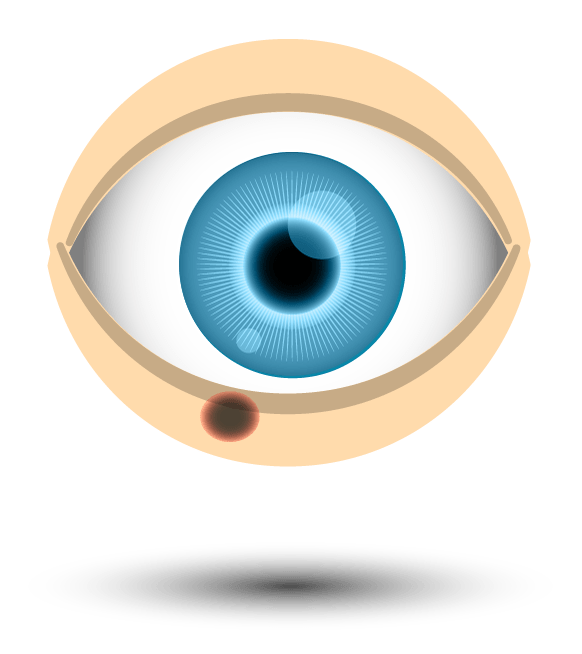
Eyelid skin cancers can present in many different shapes, sizes and colours on the eyelid, which is why it is important to always seek medical attention if you see any changes in your eyelids.
BCC skin cancers will most often present as a new lump on the eyelid. This lump is often round and red in colour and may bleed or itch at times. It does not usually have any pigment (darkening) to it, like a freckle or mole will have. Less commonly, the BCC will present as a thickening of the skin of the eyelid, which may be mistaken for a scar or a non-cancerous skin condition.
SCC skin cancers may also present as a lump or thickening and are difficult to tell apart from BCC unless a biopsy is done.
Melanomas most often present as a pigmented (dark) lump on the eyelid (like a mole), which changes rapidly in size and colour with time.
It is important to remember that:
- Eyelid skin cancers are usually painless.
- They do not usually affect the eye or vision until the advanced stages of cancer.
As with any skin cancer on the body, the earlier an eyelid skin cancer is diagnosed and treated, the better the chances for cure.
An eyelid skin cancer can often be diagnosed based on its appearance in the eyelid, but a biopsy (tissue sampling) is generally recommended to confirm that it is a skin cancer and which skin cancer it is.
An eyelid biopsy is performed under local anaesthetic in our dedicated procedure room. A small sample of the abnormal area is taken and sent to the pathology laboratory for assessment. An appointment is made within a couple of weeks to follow up and discuss results with you.
If the biopsy confirms that there is an eyelid skin cancer present, further surgery will be required to remove the cancer in full and achieve cure.
Patient information for biopsy of periocular region or eyelids with Peel Vision
The main treatment of eyelid skin cancers is surgery. The aim of surgery is to completely remove all skin cancer to reduce the risk of it coming back again in the future. The type of surgery that is chosen will depend on the type of skin cancer, the size and shape, its location in the eyelid, and whether it is primary (first-time) cancer or recurrent cancer.
There are 2 parts to any eyelid surgery for skin cancer. The first part is to completely remove the cancer from the eyelid. The second part is to reconstruct the eyelid so that it looks and functions as normally as possible.
If the skin cancer is small, then it may be possible to remove and reconstruct the eyelid in one procedure on the same day. Larger or more complex skin cancers may require a 2-part procedure (Mohs Surgery) where the cancer is removed on one day and the eyelid is reconstructed 1-3 days later. This allows the excised cancer to be assessed in the laboratory to ensure that it has been completely removed before the eyelid is reconstructed. Both the excision and reconstruction are still performed as day procedures in hospital.
Skin cancer surgery
Mohs surgery is a highly specialised form of treatment for skin cancers of the eyelid that occurs in 2 parts, with 2 separate surgeons and in 2 separate hospitals. Mohs surgery gives the highest cure rates for eyelid skin cancers whilst preserving as much normal tissue as possible around the eyelid.
Dr Then has a team of Mohs surgeons that work seamlessly with Peel Vision to coordinate this complex surgery.
- Removal of the skin cancer (Part 1).
This is performed by a team of dermatologists who have worked with Dr Then for many years to refine this complex surgery. This first part will occur in the dermatologist’s preferred day-hospital. Here, the dermatologist surgeon will remove the eyelid skin cancer under local anaesthetic and immediately examine the specimen under the microscope to ensure it has been completely removed. Sometimes more than one excision is required on the same day until the Mohs surgeon is satisfied that the cancer has been completely removed. Once removed, an eye pad is placed over the eyelid and the patient will go home.
The patient will then see Dr Then, usually 1-2 days later, at a different hospital for part 2 of the Mohs surgery, which is the reconstruction of the eyelid.
- Eyelid reconstruction (Part 2)
Dr Then will reconstruct the eyelid following the removal of the skin cancer. How this is done will depend on many factors, including the size and location of the defect, and whether any vital structures (such as the tear ducts) are involved. Dr Then will discuss this with the patient prior to the reconstruction being performed. This surgery is usually day surgery and may be performed under local anaesthetic or general anaesthetic depending on how complex the surgery is. The anaesthetic chosen is to make the patient experience as stress-free and comfortable as possible.
The aim of reconstructive surgery is to achieve an eyelid that looks and functions as normally as possible.
Yes, there are. These include:
- Radiotherapy
- Cryotherapy (freezing)
- Skin Creams (eg Aldara, Efudex)
These treatments are generally reserved for patients in whom surgery is contraindicated (elderly, frail, very unwell patients), or in patients with very early, very superficial skin cancers as the cure rates with these are not as good as with surgery.
This will vary between patients and will depend on the extent and type of surgery required to reconstruct the eyelid. Dr Then will guide each patient individually through their recovery process.
In most cases, an eye pad will be worn over the eyelid for 3-5 days after the reconstruction, then removed. There will be bruising and swelling over the reconstructed site for the first few weeks after surgery. There may be some discomfort which is usually controlled with simple pain-killers such as paracetamol and ibuprofen.
The aim of treatment is to completely remove any tumour from the eyelid. With Mohs surgery, the rates of recurrence are very low but not zero.
If microscopic tumour cells are left behind, this may lead to recurrence of the cancer, which can occur months to years later. Recurrent tumours may grow slowly under the skin and be difficult to diagnose under the scar of the first surgery or treatment. Recurrent skin cancers also tend to be more aggressive and more difficult to treat.
It is therefore important that any patient with any eyelid tumour is monitored regularly after surgery. Dr Then will usually see you regularly in the first year after surgery, and then less frequently after that, to check your eyelids for any tumour recurrence. This is usually for a total period of 5 years for most eyelid skin cancers.
With private health insurance cover, most of the cost for both excision and reconstruction will be covered by your health fund. There may still be a gap for the procedure however this is capped or limited where possible to reduce your out-of-pocket expense. You will be provided with a quote of any expected cost for the type of surgery expected before proceeding with surgery. However, the type of reconstructive surgery required may change following excision of the cancer. If this happens, you will be notified immediately of any change to cost.
Without private health cover, the reconstruction may be covered by Medicare if you meet the criteria for public surgery at Peel Health Campus. However, you will have full out-of-pocket costs for the dermatologist completing the excision of the cancer. This is quoted for you prior to proceeding with any surgery.